Exemplary Professional Practice

Every day, nurses at Children’s Health expand and nurture their role with patients, families, the community and team members. They demonstrate their commitment to professional nursing by applying new evidence to drive innovative best practices that improve their workplace and enhance children’s lives. In 2022, our nurses applied new knowledge by:
- Launching an RN clinical coach model to advance cardiac clinical nursing care
- Reducing pressure injuries in the pediatric intensive care unit
- Standardizing evidence-based prevention techniques for central line-associated bloodstream infections (CLABSIs) in the cancer center
- Reducing incidents of workplace violence through consultation of clinical nurse experts
Coaching to Enhance Proactive Thinking and Advance Clinical Care
Research shows that surgical mortality for inpatients in pediatric cardiac care is significantly impacted when more than 20% of nursing staff have less than two years of experience. As our overall RN experience level began to decrease in the Cardiac Intensive Care Unit (CICU), nurse leaders developed a new clinical coach model to advance new nurse competency and critical thinking skills.
The model’s goals:
- Accelerate newer nurses’ clinical reasoning and decision-making
- Retain highly skilled, expert nurses at the bedside
Coached staff quickly began to see the personalized, in-depth training gave them a deeper understanding of complex patient anatomy and physiology, allowing them to anticipate clinical changes and respond quickly. After the traditional, intense, nurse residency orientation to CICU, graduate nurses are paired with a coach for one shift every three months for their first three years.
“Our inpatients are sicker and more fragile than ever before. Proactive coaching accelerates how quickly new nurses recognize the subtle signs of patient deterioration. It’s also a great source of pride for our experienced nurses to help them on this journey.”
Coaches plan their shifts in advance, shaping the day according to nurse need and patient acuity. Coaches also focus on junior preceptors and nurses new to high-risk modalities, such as ventricular assist devices and renal replacement therapy. Surveys reveal an increase in nurse-reported preparedness to effectively care for patients and increased confidence at the bedside. Turnover has been significantly reduced, and experienced nurses appreciate a chance to advance in their career without moving away from direct patient care. This innovative coach program is being spread to the other critical care areas.
Reducing HAPIs in PICU Patients
Guidelines call for pediatric intensive care unit (PICU) patients to be turned every two hours. However, critically ill and unstable patients can respond poorly to being repositioned. The organization saw rates of serious hospital-acquired pressure injuries (HAPIs) increasing and sought to understand why. Personal observation by a senior nurse and surveys indicated nurses and doctors sometimes avoided or delayed turning routines due to fears of clinical deterioration in an unstable patient.
An interdisciplinary team of nurses, doctors, physical and occupational therapists, and wound care specialists conducted a literature review.
“There is lots of pressure on nurses to decrease pressure injuries, but not much in the literature specific to high-risk pediatric patients. Our interdepartmental team is changing that.”
The HAPI team developed a clinical practice guideline based on their combined expertise and evidence adapted from the literature on adult patients. A short trial allowed the guidelines to be fine-tuned after PICU nurse feedback before full-scale adoption. The nurses now feel empowered to discuss medically unstable patients during daily rounds, suggesting strategies to decrease HAPIs proactively.
All PICU staff are trained in the new guidelines and partner on safe, smaller repositioning techniques rather than full turns when a patient is unstable. A video was created to demonstrate various methods and tools nurses and physical therapists can use for smaller repositioning.
Best-In-Class CLABSI Prevention
Approximately 80% of Children’s Health oncology and stem cell transplant patients have an indwelling central line. Central lines allow the clinical team to obtain the necessary lab work to evaluate a child's condition and to safely and effectively infuse medications, such as chemotherapy.
Every time a central line is accessed, there’s an opportunity to prevent or introduce an infection risk. For the last three years, the central line-associated bloodstream infection (CLABSI) rate for the Pauline Allen Gill Center for Cancer and Blood Disorders outperformed the national average by 50%.
These outstanding results are the product of a multi-year effort by the nursing team to build tools, checklists and processes for accountable behaviors that minimize CLABSI infections. During 2021 and 2022, this team added regular observations by a dedicated central line nurse to validate competency for all nurses, including new graduates and temporary agency nurses.
The dedicated central line nurse conducts clinical surveillance rounds on patients, provides real-time coaching to team members on central line management and unique dressings, and performs audits to ensure CLABSI best practice adherence. This dedicated nursing resource also educates families on ways to reduce infection risks.
“We hypothesized that everyone was following protocols and using the CLABSI bundle accurately and correctly, given our results. This year we verified that evidence-based nursing interventions are making the difference.”
Reducing Workplace Violence and Improving Patient Safety

Like all pediatric hospitals in the United States, Children’s Health nurses experienced higher rates of abuse, assaults and harassment from patients in 2021. A lack of child and adolescent mental health care was exacerbated during the COVID-19 pandemic, leaving lasting effects on our youth. On top of this, our nurses were seeing more inpatients with increased behavioral health concerns in conjunction with comorbidities, such as asthma, diabetes or cystic fibrosis.
Nursing staff feedback revealed that current methods of patient management were not effective enough to address this growing population of patients.
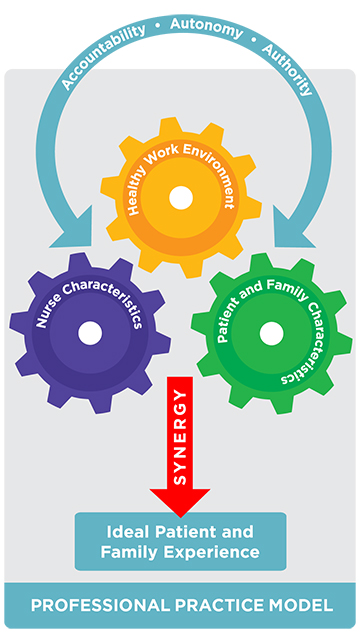
Children’s Health surveyed nurses about their top concerns in caring for patients with mental health needs, then tailored a rapid response to address those concerns using our Professional Practice Model for Nursing.
First, a new role, psychiatric resource nurse, was created and filled from the existing psychiatry teams. They provide real-time, in-person support and training upon a nurse’s request for a consult. They also connect medical patients and clinical nurses with the Behavioral Emergency Response Team (BERT) and coach nurses new to the complex charting of behavioral issues.
Literature shows that adverse childhood experiences can negatively affect how pediatric patients respond to stress and hospitalization. These expert psychiatric RNs focus on de-escalating a patient’s behavior through real-time demonstration of evidence-based best practices in intervention strategies and techniques.
This new role was overwhelmingly successful, decreasing the nurse assault rate (including patient hitting, punching, slapping, biting and kicking) from 2021 to 2022. Nurses report feeling more confident in de-escalating strategies and greater knowledge of in-house and community resources available for their patients and themselves.
- We’re growing in Dallas and Plano!
- View our nursing jobs